Gender Medicine Monthly
April - May 2023
This is the 2nd edition of my new newsletter Gender Medicine Monthly, dedicated to sharing updates related to gender medicine with a particular focus on pediatric gender medicine and the affirmative model of care, for paying subscribers.
March’s inaugural issue is free, as well as a preview of the first part of this issue. If you find the content of this newsletter valuable, please consider becoming a paid subscriber. Your support helps me dedicate my time and energy to producing quality content.
Here are some headlines and updates in gender medicine from April covered in this edition of Gender Medicine Monthly.
The AAP dodged my emails about a new Resolution submitted March 31
Sweden published a systematic evidence review on “gender-affirming care” and concluded that it should not be standard practice
New academic paper debunks arguments frequently made in support of “gender-affirming care”
New study finds no mental health benefits of social transition
New bill explicitly excludes detransition care
Former Tavistock psychotherapist echoes concerns that led to its closure in new op-ed
Jesse Singal debunks Dr. Marci Bowers’ NYT fluff piece on gender medicine
Missouri Attorney General issued an emergency regulation heavily restricting pediatric medical transition services
Jubilee hosts a debate between detransitioners and trans-identified adults
1. The AAP dodged my emails about a new Resolution that was submitted March 31
A new Resolution was submitted to the American Academy of Pediatrics requesting a systematic evidence review of “gender-affirming care” on March 31, 2023. Last month, I sent five emails to various media contacts at the AAP asking what steps they plan to take in response to the Resolution. I got no reply.
Media representative Lisa Black responded promptly to an email from a colleague of mine regarding a different topic, but ignored two emails from me.
Last year, when a similar Resolution was submitted, AAP leadership invented a “new rule” that specifically disallowed pediatrician comments on it, and omitted it from a list of other Resolutions that was emailed to members to comment on.
Their original policy statement in support of the gender-affirming model of care was written in 2018 by Dr. Jason Rafferty and represents the official position of the AAP — although it does not appear to have been reviewed by anyone else at the organization. Rafferty was responsible for conceptualizing, drafting, reviewing, revising, and approving the manuscript himself, according to a note at the end of the paper.
In the statement, Rafferty aimed to equate the clinical approach of "watchful waiting" with the discredited practice of "conversion therapy," without evidence to support the equation. Rafferty's three reasons for rejecting watchful waiting were debunked by Dr. James Cantor, who pointed out that Rafferty ignored the consistent findings of 11 studies on desistance and provided no serious evidence to support his preference for "affirmation" in childhood. Rafferty's equation of "watchful waiting" with "conversion therapy" was based entirely on studies on homosexuality, and some of the sources he cited in support of affirmation actually endorsed "watchful waiting.”
I am still holding out hope for the AAP, as last month AAP representatives told the British Journal of Medicine that all policy statements are reviewed after five years and so a “revision is under way.”
2. Sweden published a systematic evidence review on “gender-affirming care” and concluded that it should not be standard practice
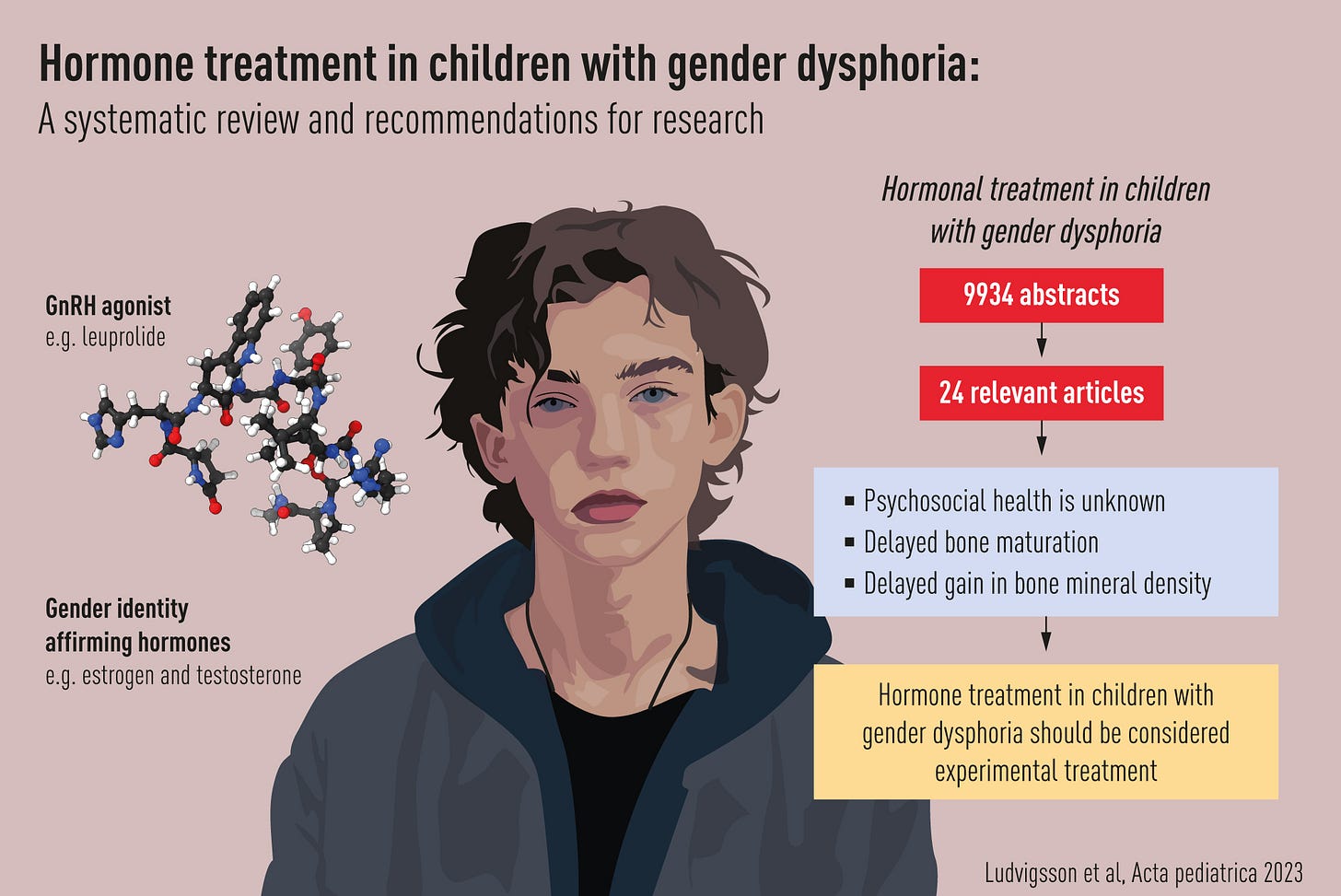
Source: Acta Paediactrica 4/17/23
Swedish researchers conducted a systematic evidence review to see what we know about giving puberty blockers and cross-sex hormones to kids under 18 with gender dysphoria. They found that we don't have enough information about how hormones affect kids' mental health, but there is some evidence that it may affect bone growth. Since there aren't enough studies that are good quality, we can't tell what the long-term effects of hormone treatment on mental health are.
The study recommends that hormone treatment for kids with gender dysphoria should only be given as part of a research study with informed consent, because we still need to learn more about it. The study also suggests that we need more research that follows patients for a long time, as the few long-term studies they did find had small sample sizes and a high dropout rate. The researchers created a checklist to help future studies in this area be better quality.
Significance: A systematic evidence review is considered one of the highest levels of evidence in the hierarchy of evidence-based research. It is a rigorous process of identifying, appraising, and synthesizing all available evidence on a specific research question, using a standardized methodology to minimize bias and error. Systematic reviews are considered highly reliable because they provide a comprehensive and unbiased summary of all available evidence on a specific topic, and can help inform healthcare decision-making by identifying the most effective treatments or interventions based on the best available evidence.
Recall from the last issue of Gender Medicine Monthly that the pioneers of the evidence-based medicine (EBM) movement said the current guidelines for managing gender dysphoria in adolescents in the US are “untrustworthy” and not evidence-based.
Progressive European countries like Finland, Sweden, the UK, and the state of Florida have conducted systematic evidence reviews and abandoned the “gender-affirming” model of care, while US-based medical organizations still have not conducted systematic evidence reviews, and are actively resisting calls to do so.